A risk register can be described as a log or repository of the various risk assessments and control performed within an organization. It is a dynamic document which enables the organization to understand its comprehensive risk profile. It provides a structure for collecting information about risks that will assist both in the analysis of risks and in decisions about whether or how these risks should be controlled, managed and monitored.
Institute News
- Woman inner peace and family general health seminar announcement
- The 2nd Conference of Medical Biophysics and its Applications
- Handwashing awareness
- 6th october artistic and cultural competition announcement
- leukemia Awareness Month Sceitific day
- Students Orientation Autumn 2025/26
- 6th October celebration
Students News
- GraphPad Prism as a statistical tool for biomedica...
- Tools of References Management " EndNote "
- MRI Postgraduate application procedures
- Exam Schedule Spring 2025
- The Fourth Student Conference of the Medical Resea...
- Announcement for new students, registration spring...
- Important notice for graduate students
Conferences
Failure mode effect analysis (FMEA)
FMEA is the analysis of a process to identify the possible ways it might fail (failure mode), the effects of these failures, and possible causes of these failures.
FMEA steps
- Form of a multidisciplinary team
- Select a high risk process for analysis
- Describe and map the process
- Identify ways in which the process could fail (fail to perform its desired function)
- Identify the possible effects of each failure
- Identity any controls already in place for failure detection
- Prioritize the various failures identified
- Determine causes of failures identified
- Redesign the process to minimize the risk of failures and their effects on patients
- Pilot, implement, and audit the redesigned process
Step 1Multidisciplinary Team
To guarantee a successful outcome from FMEA the formation of a multidisciplinary team is essential. Keep the number small around 5 – 7 individuals. Teams usually include physicians, nurses, risk managers or patient safety managers in addition to any other specialty related to the process to be analyzed. Pharmacists when dealing with medication safety, surgeons when dealing with surgical safety, blood bank technicians when dealing with blood transfusion safety, etc.
Step 2Selecting the process
The process is usually chosen from hospital information on adverse or sentinel events or from recommendations produced by patient safety organizations (see risk identification).
Step 3Map the process
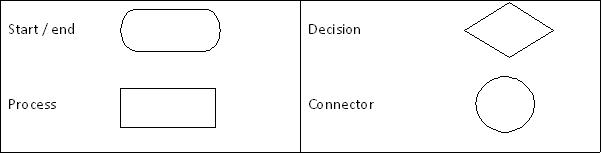
It is essential for the success of FMEA that all members of the team understand the process to be analyzed. In doing so, the process is traced from its point of initiation until its completion. It is also advisable to break down the process into its components parts. Skills related to drawing flow charts are most helpful in this step. Below are some basic shapes that are used in the construction of a flow chart.
Step 4Failure Mode
Evaluate each component of the process and determine what could go wrong with the related process. This step can be done through a series of “What if” questions and brainstorming between team members in order to define the various potential failures in the process and how often do they occur (see risk analysis).
Step 5Effect Analysis
The effects of each failure have to be determined and their impact on patients or the organization defined (see risk analysis).
Step 6Controls
The same is performed for the identification of any controls or safeguards already in place that help in the detection of each failure mode identified (see risk analysis).
FMEA sheet I can be used with step 4 to step 6.
Step 7Prioritization
Prioritize the failure modes identified using the criticality index (see risk evaluation and FMEA sheet II) to identify those that pose the greatest threat to patients or the organization. If a large number of failure modes are identified, it is more effective to address the highest rated failure modes initially. The rest of failure modes are addressed later in descending order. Solutions to the failure modes with the high ranking may be also solutions to less significant failure modes. Some organizations establish a “cut-off” criticality index to establish which failure modes will be addressed.
Step 8Causes
Determine through open discussion possible causes and predisposing factors for the identified failures. The use of Reason’s error diagram or a fish bone diagram may help in the analysis.
Step 9Improvement
For each failure mode selected identify actions required to decrease the corresponding criticality index which should lead to one or more of the following:
- Decrease the likelihood of the failure to occur
- Minimize harm resulting from the failure
- Increase probability of its detection before reaching the patient
Step 10PDSA cycle
Once improvement steps have been identified an action plan is developed to implement the suggested improvements. Before full scale implementation it is advisable to pilot the new action plan. After full scale implementation data is recollected and analyzed to make sure that the improvements introduced have lead to an increase in the process safety (decrease in Criticality Index).
Risk management tools
There are many tools that can be used for effective risk management as shown in the table.
| Risk Management Tools Risk management facilitation methods (flow charts, check sheets, etc) Failure Mode Effects Analysis Healthcare Failure Mode effects Analysis Failure Mode Effects and Critically Analysis Hazard Analysis and Critical Control Points Hazard Operability Analysis Preliminary Hazard Analysis Barrier analysis and risk controls Supporting statistical tools |
Risk register